Cardiorespiratory Adaptation
Cardiovascular Responses to Acute Exercise
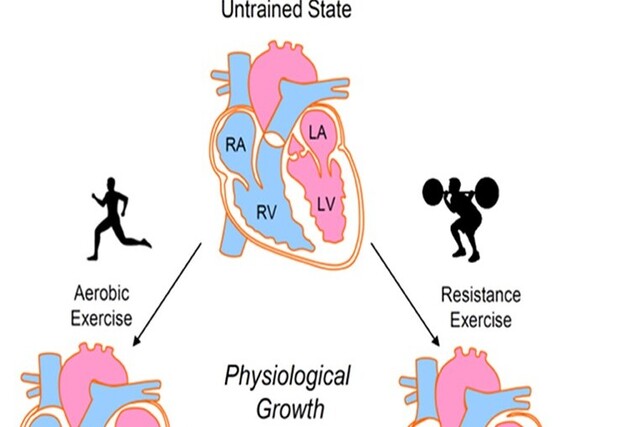
Numerous interrelated cardiovascular changes occur during dynamic exercise. The primary goal of these adjustments is to increase blood flow to working muscle; however, cardiovascular control of virtually every tissue and organ in the body is also altered. To better understand the changes that occur, we must examine the function of both the heart and the peripheral circulation.
In this section we examine changes in all components of the cardiovascular system from rest to acute exercise, looking specifically at the following: • Heart rate • Stroke volume • Cardiac output • Blood pressure • Blood flow • The blood
We then see how these changes are integrated to maintain adequate blood pressure and provide for the exercising body’s needs.
Heart Rate
Heart rate (HR) is one of the simplest physiological responses to measure, and yet one of the most informative in terms of cardiovascular stress and strain. Measuring HR involves simply taking the subject’s pulse, usually at the radial or carotid artery. Heart rate is a good indicator of relative exercise intensity.
Resting Heart Rate
Resting heart rate (RHR) averages 60 to 80 beats/min in most individuals. In highly conditioned, endurance-trained athletes, resting rates as low as 28 to 40 beats/min have been reported. This is mainly due to an increase in parasympathetic (vagal) tone that accompanies endurance exercise training. Resting heart rate can also be affected by environmental factors; for example, it increases with extremes in temperature and altitude. Just before the start of exercise, preexercise HR usually increases above normal resting values. This is called the anticipatory response. This response is mediated through release of the neurotransmitter norepinephrine from the sympathetic nervous system and the hormone epinephrine from the adrenal medulla. Vagal tone also decreases. Because preexercise HR is elevated, reliable estimates of the true RHR should be made only under conditions of total relaxation, such as early in the morning before the subject rises from a restful night’s sleep.”
Heart Rate During Exercise
When exercise begins, HR increases directly in proportion to the increase in exercise intensity , until near-maximal exercise is achieved. As maximal exercise intensity is approached, HR begins to plateau even as the exercise workload continues to increase. This indicates that HR is approaching a maximal value. The maximum heart rate (HRmax) is the highest HR value achieved in an all-out effort to the point of volitional fatigue. Once accurately determined, HRmax is a highly reliable value that remains constant from day to day. However, this value changes slightly from year to year due to a normal age-related decline.
HRmax is often estimated based on age because HRmax shows a slight but steady decrease of about one beat per year beginning at 10 to 15 years of age. Subtracting one’s age from 220 beats/min provides a reasonable approximation of one’s predicted HRmax. However, this is only an estimate—individual values vary considerably from this average value. To illustrate, for a 40-year-old woman, HRmax would be estimated to be 180 beats/min (HRmax = 220 – 40 beats/min). However, 68% of all 40-year-olds have actual HRmax values between 168 and 192 beats/min (mean ± 1 standard deviation), and 95% fall between 156 and 204 beats/min (mean ± 2 standard deviations). This demonstrates the potential for error in estimating a person’s HRmax. A similar but more accurate equation has been developed to estimate HRmax from age. In this equation, HRmax = 208 – (0.7 × age).
When the exercise intensity is held constant at any submaximal workload, HR increases fairly rapidly until it reaches a plateau. This plateau is the steady-state heart rate, and it is the optimal HR for meeting the circulatory demands at that specific rate of work. For each subsequent increase in intensity, HR will reach a new steady-state value within 2 to 3 min. However, the more intense the exercise, the longer it takes to achieve this steady-state value.
The concept of steady-state heart rate forms the basis for simple exercise tests that have been developed to estimate cardiorespiratory (aerobic) fitness. In one such test, individuals are placed on an exercise device, such as a cycle ergometer, and then perform exercise at two or three standardized exercise intensities. Those with better cardiorespiratory endurance capacity will have a lower steady-state HR at each exercise intensity than those who are less fit. Thus, a lower steady-state HR at a fixed exercise intensity is a valid predictor of greater cardiorespiratory fitness.
Stroke Volume
Stroke volume (SV) also changes during acute exercise to allow the heart to meet the demands of exercise. At near-maximal and maximal exercise intensities, as heart rate approaches its maximum, SV is a major determinant of cardiorespiratory endurance capacity. Stroke volume is determined by four factors:
- The volume of venous blood returned to the heart (the heart can only pump what returns)
- Ventricular distensibility (the capacity to enlarge the ventricle, to allow maximal filling)
- Ventricular contractility (the inherent capacity of the ventricle to contract forcefully)
- Aortic or pulmonary artery pressure (the pressure against which the ventricles must contract)
The first two factors influence the filling capacity of the ventricle, determining how much blood fills the ventricle and the ease with which the ventricle is filled at the available pressure. Together, these factors determine the end-diastolic volume (EDV), sometimes referred to as the preload. The last two characteristics influence the ventricle’s ability to empty during systole, determining the force with which blood is ejected and the pressure against which it must be expelled into the arteries. The latter factor, the aortic mean pressure, which represents resistance to blood being ejected from the left ventricle (and to a less important extent, the pulmonary artery pressure resistance to flow from the right ventricle), is referred to as the afterload. These four factors combine to determine the SV during acute exercise.
Stroke Volume Increase With Exercise Stroke volume increases above resting values during exercise. Most researchers agree that SV increases with increasing exercise intensity up to intensities somewhere between 40% and 60% of V . O2max. At that point, SV typically plateaus, remaining essentially unchanged up to and including the point of exhaustion. However, other researchers have reported that SV continues to increase beyond 40% to 60% V . O2max, even up through maximal exercise intensities.
When the body is in an upright position, SV can approximately double from resting to maximal values. For example, in active but untrained individuals, SV increases from about 60 to 70 ml/beat at rest to 110 to 130 ml/beat during maximal exercise. In highly trained endurance athletes, SV can increase from 80 to 110 ml/beat at rest to 160 to 200 ml/beat during maximal exercise. During supine exercise, such as recumbent cycling, SV also increases but usually by only about 20% to 40%—not nearly as much as in an upright position.
Why does body position make such a difference? When the body is in the supine position, blood does not pool in the lower extremities. Blood returns more easily to the heart in a supine posture, which means that resting SV values are higher in the supine position than in the upright position. Thus, the increase in SV with maximal exercise is not as great in the supine position as in the upright position because SV starts out higher. Interestingly, the highest SV attainable in upright exercise is only slightly greater than the resting value in the reclining position. The majority of the SV increase during low to moderate intensities of exercise in the upright position appears to be compensating for the force of gravity that causes blood to pool in the extremities.
Explanations for the Stroke Volume Increase One explanation for the increase in SV with exercise is that the primary factor determining SV is increased preload or the extent to which the ventricle fills with blood and stretches, that is, the EDV. When the ventricle stretches more during filling, it subsequently contracts more forcefully. For example, when a larger volume of blood enters and fills the ventricle during diastole, the ventricular walls stretch to a greater extent. To eject that greater volume of blood, the ventricle responds by contracting more forcefully. This is referred to as the Frank-Starling mechanism. At the level of the muscle fiber, the greater the stretch of the myocardial cells, the more actin-myosin cross-bridges formed, and greater force is developed.
Additionally, SV will increase during exercise if the ventricle’s contractility (an inherent property of the ventricle) is enhanced. Contractility can increase by increasing sympathetic nerve stimulation or circulating catecholamines (epinephrine, norepinephrine), or both. An improved force of contraction can increase SV with or without an increased EDV by increasing the ejection fraction. Finally, when mean arterial blood pressure is low, SV is greater since there is less resistance to outflow into the aorta. These mechanisms all combine to determine the SV at any given intensity of dynamic exercise.
Measuring Stroke Volume Stroke volume is much more difficult to measure than HR. Some clinically used cardiovascular diagnostic techniques have made it possible to determine exactly how SV changes with exercise. Echocardiography (using sound waves) and radionuclide techniques (“tagging” of red blood cells with radioactive tracers) have elucidated how the heart chambers respond to increasing oxygen demands during exercise. With either technique, continuous images of the heart can be taken at rest and up to near-maximal intensities of exercise.
Recall that HR also increases with exercise intensity. The plateau or small decrease in left ventricular EDV at high exercise intensities could be caused by a reduced ventricular filling time due to the high HR. One study showed that ventricular filling time decreased from about 500 to 700 ms at rest to about 150 ms at HRs between 150 and 200 beats/min. Therefore, with increasing intensities approaching V . O2max (and HRmax), the diastolic filling time could be shortened enough to limit filling. As a result, EDV might plateau or even start to decrease.
For the Frank-Starling mechanism to increase SV, left ventricular EDV must increase, necessitating an increased venous return to the heart. The muscle pump and respiratory pump both aid in increasing venous return. In addition, redistribution of blood flow and volume from inactive tissues such as the splanchnic and renal circulations increases the available central blood volume.
To review, three factors that contribute to an increase in SV with increasing intensity of exercise are increased venous return (preload), increased ventricular contractility, and decreased afterload resulting from a decrease in total peripheral resistance due to vasodilation of the blood vessels in exercising skeletal muscle.
Cardiac Output Since cardiac output is the product of heart rate and stroke volume (Q . = HR SV), cardiac output predictably increases with increasing exercise intensity . Resting cardiac output is approximately 5.0 L/ min but varies in proportion to the size of the person. Maximal cardiac output varies between less than 20 L/ min in sedentary individuals to 40 or more L/min in elite endurance athletes. Maximal Q . is a function of both body size and endurance training. The linear relationship between cardiac output and exercise intensity is expected because the major purpose of the increase in cardiac output is to meet the muscles’ increased demand for oxygen. Like V . O2max, when cardiac output approaches maximal exercise intensity it may reach a plateau. In fact, it is likely that V . O2max is ultimately limited by the inability of cardiac output to increase further.
The Integrated Cardiac Response to Exercise To see how HR, SV, and Q . vary under various conditions of rest and exercise, consider the following example. An individual first moves from a reclining position to a seated posture and then to standing. Next the person begins walking, then jogging, and finally breaks into a fast-paced run. How does the heart respond? In a reclining position, HR is ~50 beats/min; it increases to about 55 beats/min during sitting and to about 60 beats/min during standing. When the body shifts from a reclining to a sitting position and then to a standing position, gravity causes blood to pool in the legs, which reduces the volume of blood returning to the heart and thus decreases SV. To compensate for the reduction in SV, HR increases in order to maintain cardiac output; that is, Q = HR X SV. During the transition from rest to walking, HR increases from about 60 to about 90 beats/min. Heart rate increases to 140 beats/min with moderate-paced jogging and can reach 180 beats/min or more with a fast-paced run. The initial increase in HR—up to about 100 beats/min—is mediated by a withdrawal of parasympathetic (vagal) tone. Further increases in HR are mediated by increased activation of the sympathetic nervous system. Stroke volume also increases with exercise, further increasing cardiac output. These relationships are illustrated in
Blood Pressure
During endurance exercise, systolic blood pressure increases in direct proportion to the increase in exercise intensity. However, diastolic pressure does not change significantly and may even decrease. As a result of the increased systolic pressure, mean arterial blood pressure increases. A systolic pressure that starts out at 120 mmHg in a normal healthy person at rest can exceed 200 mmHg at maximal exercise. Systolic pressures of 240 to 250 mmHg have been reported in normal, healthy, highly trained athletes at maximal intensities of aerobic exercise. Increased systolic blood pressure results from the increased cardiac output (Q . ) that accompanies increasing rates of work. This increase in pressure helps facilitate the increase in blood flow through the vasculature. Also, blood pressure (that is, hydrostatic pressure) in large part determines how much plasma leaves the capillaries, entering the tissues and carrying needed supplies. Thus increased systolic pressure aids substrate delivery to working muscles.
After increasing initially, mean arterial pressure reaches a steady state during submaximal steady-state endurance exercise. As work intensity increases, so does systolic blood pressure. If steady-state exercise is prolonged, the systolic pressure might start to decrease gradually, but diastolic pressure remains constant. The slight decrease in systolic blood pressure, if it occurs, is a normal response and simply reflects increased vasodilation in the active muscles, which decreases the total peripheral resistance, or TPR (since mean arterial pressure = cardiac output total peripheral resistance). Diastolic blood pressure changes little during submaximal dynamic exercise; however, at maximal exercise intensities, diastolic blood pressure may increase slightly. Remember that diastolic pressure reflects the pressure in the arteries when the heart is at rest (diastole). With dynamic exercise there is an overall increase in sympathetic tone to the vasculature, causing overall vasoconstriction. However, this vasoconstriction is blunted in the exercising muscles by the release of local vasodilators, a phenomenon called sympatholysis. Thus, because there is a balance between vasoconstriction to inactive regional circulations and vasodilation in active skeletal muscle, diastolic pressure does not change substantially. However, in some cases of cardiovascular disease, increases in diastolic pressure of 15 mmHg or more occur in response to exercise and are one of several indications for immediately stopping a diagnostic exercise test.
Upper body exercise causes a greater blood pressure response than leg exercise at the same absolute rate of energy expenditure. This is most likely attributable to the smaller exercising muscle mass of the upper body compared with the lower body, plus an increased energy demand needed to stabilize the upper body during arm exercise. This difference in the systolic blood pressure response to upper and lower body exercise has important implications for the heart. Myocardial oxygen uptake and myocardial blood flow are directly related to the product of HR and systolic blood pressure (SBP). This value is referred to as the rate–pressure product (RPP), or double product (RPP = HR X SBP). With static or dynamic resistance exercise or upper body work, the rate–pressure product is elevated, indicating increased myocardial oxygen demand. The use of rate–pressure product as an indirect index of myocardial oxygen demand is important in clinical exercise testing. Periodic blood pressure increases during resistance exercise, such as weightlifting, can be extreme. With high-intensity resistance training, blood pressure can briefly reach 480/350 mmHg. Very high pressures like these are more commonly seen when the exerciser performs a Valsalva maneuver to aid heavy lifts. This maneuver occurs when a person tries to exhale while the mouth, nose, and glottis are closed. This action causes an enormous increase in intrathoracic pressure. Much of the subsequent blood pressure increase results from the body’s effort to overcome the high internal pressures created during the Valsalva maneuver.
Blood Flow
Acute increases in cardiac output and blood pressure during exercise allow for increased total blood flow to the body. These responses facilitate increased blood to areas where it is needed, primarily the exercising muscles. Additionally, sympathetic control of the cardiovascular system redistributes blood so that areas with the greatest metabolic need receive more blood than areas with low demands.
Redistribution of Blood During Exercise
Blood flow patterns change markedly in the transition from rest to exercise. Through the vasoconstrictor action of the sympathetic nervous system on local arterioles, blood flow is redirected away from areas where elevated flow is not essential to those areas that are active during exercise. Only 15% to 20% of the resting cardiac output goes to muscle, but during high-intensity exercise, the muscles may receive 80% to 85% of the cardiac output. This shift in blood flow to the muscles is accomplished primarily by reducing blood flow to the kidneys and the so-called splanchnic circulation (which includes the liver, stomach, pancreas, and intestines). Because cardiac output increases greatly with increasing intensity of exercise, the values are shown both as the relative percentage of cardiac output and as the absolute cardiac output going to each regional circulation at rest and at three intensities of exercise. Although several physiological mechanisms are responsible for the redistribution of blood flow during exercise, they work together in an integrated fashion. To illustrate this, consider what happens to blood flow during exercise, focusing on the primary driver of the response, namely the increased blood flow requirement of the exercising skeletal muscles.
As exercise begins, active skeletal muscles rapidly require increased oxygen delivery. This need is partially met through sympathetic stimulation of vessels in those areas to which blood flow is to be reduced (e.g., the splanchnic and renal circulations). The resulting vasoconstriction in those areas allows for more of the (increased) cardiac output to be distributed to the exercising skeletal muscles. In the skeletal muscles, sympathetic stimulation to the constrictor fibers in the arteriolar walls also increases; however, local vasodilating substances are released from the exercising muscle and overcome sympathetic vasoconstriction, producing an overall vasodilation in the muscle (sympatholysis). Many local vasodilating substances are released in exercising skeletal muscle. As the metabolic rate of the muscle tissue increases during exercise, metabolic waste products begin to accumulate. Increased metabolism causes an increase in acidity (increased hydrogen ions and lower pH), carbon dioxide, and temperature in the muscle tissue. These are some of the local changes that trigger vasodilation of, and increasing blood flow through, the arterioles feeding local capillaries. Local vasodilation is also triggered by the low partial pressure of oxygen in the tissue or a reduction in oxygen bound to hemoglobin (increased oxygen demand), the act of muscle contraction, and possibly other vasoactive substances (including adenosine) released as a result of skeletal muscle contraction.
When exercise is performed in a hot environment, there is also an increase in blood flow to the skin to help dissipate the body heat. The sympathetic control of skin blood flow is unique in that there are sympathetic vasoconstrictor fibers (similar to skeletal muscle) and sympathetic active vasodilator fibers interacting over most of the skin surface area. During dynamic exercise, as body core temperature rises, there is initially a reduction in sympathetic vasoconstriction, causing a passive vasodilation. Once a specific body core temperature threshold is reached, skin blood flow begins to dramatically increase by activation of the sympathetic active vasodilator system. The increase in skin blood flow during exercise promotes heat loss, because metabolic heat from deep in the body can be released only when blood moves close to the skin.
Cardiovascular Drift
Cardiovascular Drift is a term used to describe a set of cardiovascular changes that occur during prolonged aerobic exercise, especially in hot or challenging environmental conditions when maintaining a steady intensity. This phenomenon reflects the body’s adaptive responses to the demands of extended physical activity and environmental stressors. One of the key features of cardiovascular drift is the gradual reduction in Stroke Volume (SV), which represents the amount of blood ejected by the heart with each contraction. This reduction in SV occurs over time during sustained exercise. As SV decreases, there is a corresponding increase in Heart Rate (HR). This compensatory increase in HR is necessary to maintain Cardiac Output (Q), which is the total volume of blood pumped by the heart per minute. Cardiac Output (Q) is calculated as the product of Heart Rate (HR) and Stroke Volume (SV). Therefore, when SV decreases, HR must rise to ensure that an adequate volume of blood continues to be pumped to meet the body’s oxygen and nutrient demands.
Despite the decrease in SV and the increase in HR, Cardiac Output (Q) remains relatively stable during cardiovascular drift. The heart adapts to the reduced blood volume ejected per beat by pumping blood more frequently. This helps maintain a consistent flow of blood to the working muscles and other vital tissues. Another characteristic of cardiovascular drift is a decline in Arterial Blood Pressure. This reduction in blood pressure is primarily linked to the redistribution of blood flow within the body. During exercise in hot conditions, there is an increased demand for heat dissipation and temperature regulation. To facilitate this, more blood is directed to the skin’s vasodilated vessels, which helps dissipate heat. However, this redirection of blood away from other areas results in a decrease in Arterial Blood Pressure.
Moreover, cardiovascular drift involves reduced Venous Return to the heart. As more blood is directed toward the skin’s vasodilated vessels for cooling purposes, less blood is available to return to the heart. Consequently, there is a decrease in End-Diastolic Volume (EDV), which represents the amount of blood in the ventricles just before they contract. With decreased EDV, Stroke Volume (SV) is further reduced. In addition to the changes in blood volume distribution, cardiovascular drift may lead to a slight decrease in Blood Volume overall. This decrease occurs due to factors such as sweating and a shift of plasma (the liquid component of blood) from the capillaries into the surrounding tissues.
Competition for Blood Supply
During exercise, the body undergoes significant changes in blood flow to meet the increased oxygen and nutrient demands of active tissues. However, there is a limit to the amount of blood that the heart can pump per minute, known as cardiac output. When exercise is added to the body’s overall blood flow demands, there can be competition for this limited cardiac output among various vascular beds or systems in the body.
The specific vascular beds that compete for available blood flow can vary depending on the circumstances. For example, competition for blood flow might occur between active skeletal muscles and the gastrointestinal system, particularly after a meal. Research conducted on miniature pigs examined the effects of feeding versus fasting on blood flow distribution during exercise. The pigs were divided into two groups: one group fasted for an extended period before exercise, while the other group consumed their morning ration in two portions, with the second portion shortly before exercise. Both groups of pigs then engaged in exercise at around 65% of their maximum oxygen consumption (V . O2max).
The results of this study showed that blood flow to the hindlimb muscles during exercise was 18% lower in the fed group compared to the fasted group. Conversely, blood flow to the gastrointestinal system was 23% higher in the fed group. Similar findings in humans suggest that after a meal, there is a reduced redistribution of blood flow from the gastrointestinal system to the working muscles during exercise. As a practical implication, this research suggests that athletes should carefully consider the timing of their meals before competition to optimize blood flow to the active muscles during exercise. Another example of competition for blood flow occurs during exercise in a hot environment. In such conditions, there can be competition between the skin’s circulation, which is responsible for thermoregulation and cooling the body, and the circulation to the exercising muscles. This competition for available cardiac output is a complex interaction that can have significant implications for exercise performance and body temperature regulation, especially in hot and challenging environments.
Blood
In addition to the heart and blood vessels, blood itself plays a crucial role in the cardiovascular system’s response to exercise. Blood is the fluid responsible for transporting oxygen and nutrients to the body’s tissues while also removing waste products generated during metabolism. As exercise increases metabolic demands, various aspects of blood become increasingly important for optimal performance.
Oxygen Content
At rest, the oxygen content in the blood ranges from 20 ml of oxygen per 100 ml of arterial blood to 14 ml of oxygen per 100 ml of venous blood returning to the right atrium of the heart. The difference between these two values (20 ml – 14 ml = 6 ml) is known as the arterial-mixed venous oxygen difference, often abbreviated as (a-v ¯)O2 difference. This value represents the extent to which oxygen is extracted or removed from the blood as it circulates through the body.
As exercise intensity increases, the (a-v ¯)O2 difference progressively rises and can nearly triple from rest to maximal exercise intensities. This increase primarily reflects a reduction in venous oxygen content because arterial oxygen content remains relatively stable from rest to maximal exertion. With higher exercise intensity, the active muscles require more oxygen, leading to increased extraction of oxygen from the blood. Consequently, the venous oxygen content decreases, approaching minimal levels in the active muscles. However, it’s important to note that mixed venous blood returning to the right atrium of the heart rarely drops below 4 ml of oxygen per 100 ml of blood. This is because the blood returning from active tissues mixes with blood from inactive tissues as it returns to the heart. Oxygen extraction by inactive tissues is significantly lower compared to active muscles.
Plasma Volume
When an individual transitions to an upright position or commences exercise, there is an immediate loss of plasma from the bloodstream to the interstitial fluid space. This fluid movement out of the capillaries is governed by various pressures within the capillaries, including hydrostatic pressure (resulting from increased blood pressure) and oncotic pressure (exerted by blood proteins, mainly albumin). Fluid movement out of the capillaries is influenced by external factors, such as tissue pressure and oncotic pressures originating from proteins in the interstitial fluid. Osmotic pressures from electrolytes in solution on both sides of the capillary wall also contribute to this process. As exercise leads to an increase in blood pressure, it elevates the hydrostatic pressure within the capillaries, prompting the movement of water from the intravascular compartment to the interstitial compartment. Additionally, as metabolic waste products accumulate in active muscles, intramuscular osmotic pressure rises, drawing fluid from the capillaries into the muscle.
Prolonged exercise can result in a significant reduction in plasma volume, typically in the range of 10% to 15%. The most substantial reductions occur during the initial minutes of exercise. During resistance training, the loss of plasma volume is directly proportional to the intensity of effort, with comparable temporary fluid losses from the vascular space of about 10% to 15%. If exercise intensity or environmental conditions lead to sweating, additional losses of plasma volume can occur. While interstitial fluid primarily provides the fluid for sweat formation, this fluid space diminishes as sweating persists. Consequently, this raises both oncotic (as proteins do not move with the fluid) and osmotic (as sweat contains fewer electrolytes than interstitial fluid) pressures in the interstitial space, driving even more plasma out of the vascular compartment into the interstitial space. While the volume of intracellular fluid cannot be directly and precisely measured, research suggests that fluid loss can occur from the intracellular compartment during prolonged exercise, and even from red blood cells, causing them to shrink.
A reduction in plasma volume can have detrimental effects on performance. During long-duration activities, particularly when dehydration and heat dissipation become issues, blood flow to active tissues may decrease to allow more blood diversion to the skin in an attempt to dissipate body heat. It’s essential to note that a reduction in muscle blood flow occurs only under dehydrated conditions and at high exercise intensities. Severe reductions in plasma volume can also increase blood viscosity, which may hinder blood flow and consequently limit the transport of oxygen, especially if the hematocrit (percentage of red blood cells in blood) exceeds 60%.
For activities lasting only a few minutes, shifts in body fluids hold little practical significance. However, as exercise duration increases, changes in body fluids and temperature regulation become crucial factors affecting performance. For athletes participating in sports like football, the Tour de France, or marathons, these physiological processes are not only important for competition but also for overall well-being. In some cases, fatalities have occurred due to dehydration and hyperthermia during or as a result of various sports activities.
Hemoconcentration
Hemoconcentration occurs when there is a reduction in plasma volume. In this situation, the cellular and protein components of blood make up a larger proportion of the total blood volume, resulting in increased concentration. Specifically, the concentration of red blood cells can rise significantly, sometimes by as much as 20% to 25%. This can lead to an increase in hematocrit levels, which can go from 40% to 50%. Importantly, while the total number and volume of red blood cells do not undergo substantial changes, the concentration of red blood cells per unit of blood increases, indicating a higher concentration of cells. As a consequence of this hemoconcentration, the per-unit hemoglobin content in the blood also increases significantly. This elevation in hemoglobin content enhances the blood’s ability to carry oxygen, which is advantageous during exercise and provides a notable advantage at high altitudes.
Integration of the Exercise Response
The cardiovascular system undergoes various complex changes during exercise to ensure the delivery of oxygen to meet the demands of active muscles. Key areas and responses are identified and summarized to illustrate the coordination of these intricate control mechanisms. It’s essential to understand that while the body strives to meet the blood flow requirements of muscles during exercise, it can only do so if arterial blood pressure remains within an acceptable range. Maintenance of arterial blood pressure is considered the highest priority for the cardiovascular system, regardless of exercise, environmental conditions, or competing physiological needs.
Pulmonary Ventilation During Dynamic Exercise
The commencement of exercise triggers an immediate increase in ventilation. This surge in breathing often starts even before the onset of muscle contractions, indicating an anticipatory response. The rapid onset of this initial respiratory response is believed to be predominantly neural in nature, governed by the respiratory control centers in the brain (central command). Nevertheless, neural signals originating from receptors in the active muscles also contribute to this response.
The more gradual second phase of increased respiration, particularly noticeable during heavy exercise is primarily controlled by alterations in the chemical composition of arterial blood. As exercise continues, the heightened metabolic activity in muscles results in the production of more carbon dioxide (CO2) and hydrogen ions (H+). It’s important to recall that these changes shift the oxyhemoglobin saturation curve to the left, promoting oxygen unloading within the muscles and subsequently increasing the arterial-mixed venous oxygen difference (O2 difference).
Chemoreceptors that detect increased CO2 and H+ concentrations in the blood are primarily situated in the brain, carotid bodies, and lungs. These chemoreceptors then stimulate the inspiratory center in the brain, leading to an elevation in both the rate and depth of respiration. It’s worth noting that chemoreceptors within the exercising muscles themselves may also play a role in this process. Additionally, receptors in the right ventricle of the heart relay information to the inspiratory center, allowing increased cardiac output to activate breathing during the initial minutes of exercise. These collective influences of blood CO2 and H+ concentrations on breathing rate and pattern fine-tune the neural-driven respiratory response to exercise, ensuring precise alignment between oxygen delivery and aerobic demands while avoiding overexertion of respiratory muscles. After the conclusion of exercise, muscle energy demands decrease almost immediately, returning to resting levels. However, pulmonary ventilation normalizes at a slower pace. While one would expect respiration to drop to resting levels within seconds if it perfectly matched tissue metabolic demands, post-exercise breathing recovery takes several minutes. This suggests that the regulation of post-exercise respiration is primarily influenced by factors such as acid-base balance, the partial pressure of dissolved carbon dioxide (PCO2), and blood temperature.
Breathing Irregularities During Exercise
The regulation of breathing during exercise ideally aims to optimize aerobic performance. However, respiratory issues during exercise can hinder overall performance.
Dyspnea: Dyspnea, the sensation of shortness of breath, is a common experience during exercise, particularly among individuals with lower aerobic fitness levels who attempt exercise at intensities that significantly elevate arterial carbon dioxide (CO2) and hydrogen ion (H+) concentrations.
Inadequate conditioning of the respiratory muscles appears to underlie the failure to reduce these stimuli during exercise. Despite a robust neural drive to increase lung ventilation, respiratory muscles can fatigue quickly and struggle to restore normal homeostasis.
Hyperventilation: Hyperventilation refers to excessive ventilation, which can occur due to the anticipation of exercise, anxiety, or certain respiratory disorders. This overbreathing leads to increased ventilation beyond what is necessary to support exercise. At rest, hyperventilation can reduce the normal alveolar and arterial PCO2 levels (typically around 40 mmHg) to approximately 15 mmHg. As arterial CO2 concentrations drop, blood pH rises, collectively diminishing the drive to breathe. Since blood leaving the lungs is nearly always around 98% saturated with oxygen, an increase in alveolar PO2 doesn’t enhance blood oxygen content. Instead, the reduced urge to breathe and the improved breath-holding capacity following hyperventilation result from carbon dioxide unloading, not increased blood oxygen levels. This is often referred to as “blowing off CO2.” Even brief episodes of deep, rapid breathing can lead to light-headedness and, in extreme cases, loss of consciousness. This phenomenon underscores the sensitivity of the respiratory system’s regulation to carbon dioxide and pH.
Valsalva Maneuver: The Valsalva maneuver is a potentially risky respiratory maneuver that frequently accompanies specific types of exercise, particularly heavy lifting. This maneuver involves:
- Closing the glottis (the space between the vocal cords).
- Increasing intra-abdominal pressure by forcefully contracting the diaphragm and abdominal muscles.
- Elevating intrathoracic pressure by forcibly contracting the respiratory muscles.
As a result of these actions, air becomes trapped and pressurized within the lungs. The high intra-abdominal and intrathoracic pressures impede venous return by collapsing the major veins, reducing the volume of blood returning to the heart. This, in turn, diminishes cardiac output and lowers arterial blood pressure. While the Valsalva maneuver can have specific applications, it can be perilous and is generally advised against.
Ventilatory Threshold: As exercise intensity escalates, there comes a point where ventilation increases disproportionately to oxygen consumption. This threshold, typically occurring around 55% to 70% of V . O2max, is termed the ventilatory threshold. Around the same intensity level as the ventilatory threshold, there’s an increase in blood lactate levels. This may arise from greater lactate production, reduced lactate clearance, or both. Lactic acid combines with sodium bicarbonate (an acid buffer) to form sodium lactate, water, and carbon dioxide. Increased carbon dioxide levels stimulate chemoreceptors that signal the inspiratory center to boost ventilation. Thus, the ventilatory threshold signifies the respiratory response to elevated carbon dioxide levels, leading to a significant surge in ventilation beyond this threshold.
Respiratory Limitations to Performance
Respiration, like any other bodily activity, demands energy. The respiratory muscles utilize most of this energy during pulmonary ventilation. At rest, these muscles account for just about 2% of the total oxygen uptake. However, as ventilation rate and depth increase, so does the energy expenditure for respiration. The diaphragm, intercostal muscles, and abdominal muscles can consume up to 11% of the total oxygen during heavy exercise and receive up to 15% of the cardiac output. Even during the recovery phase following dynamic exercise, sustained increases in ventilation require additional energy, amounting to 9% to 12% of the total post-exercise oxygen consumption.
While respiratory muscles undergo considerable strain during exercise, ventilation typically remains sufficient to prevent an increase in alveolar carbon dioxide (PCO2) or a decline in alveolar oxygen (PO2) levels during short-duration activities. Even during maximal exertion, ventilation is usually not pushed to its maximum voluntary capacity for moving air in and out of the lungs, known as maximal voluntary ventilation. However, there’s substantial evidence suggesting that during very high-intensity exercise (95-100% V . O2max), particularly in highly trained individuals, pulmonary ventilation might become a limiting factor.
In the case of heavy breathing sustained over several hours, such as during marathon running, concerns arise about glycogen depletion and fatigue of the respiratory muscles. Animal studies indicate a significant preservation of respiratory muscle glycogen compared to muscle glycogen in exercising muscles. While equivalent human data is scarce, respiratory muscles are adapted for prolonged activity compared to extremity muscles. The diaphragm, for instance, possesses two to three times more oxidative capacity, with more oxidative enzymes, mitochondria, and capillary density than other skeletal muscles.
Airway resistance and gas exchange limitations in healthy lungs typically do not restrict exercise. During physical activity, the volume of inspired air can increase dramatically, up to 20-40 times from resting levels. Airway resistance is typically maintained at near-resting levels due to airway dilation. While in untrained and moderately trained individuals, blood leaving the lungs remains highly oxygen-saturated (~98%) even during submaximal and maximal efforts, highly trained elite endurance athletes may experience exercise-induced arterial hypoxemia (EIAH) during maximal exercise. This condition results from an imbalance between lung ventilation and blood perfusion. In these cases, the respiratory system is well-suited to handle the demands of heavy breathing during both short and prolonged physical exertion. However, highly trained individuals who have extremely high oxygen demands during exhaustive exercise may encounter respiratory limitations.
For individuals with restricted or obstructed airways, the respiratory system can indeed limit performance. Conditions like asthma, characterized by bronchial tube constriction and mucous membrane swelling, result in significant ventilation resistance and shortness of breath, especially during exercise. Exercise can exacerbate asthma symptoms, although the precise mechanisms for exercise-induced airway obstruction in individuals with exercise-induced asthma remain unclear despite extensive research efforts.
Respiratory Regulation of Acid–Base Balance
During high-intensity exercise, the body produces and accumulates lactate and hydrogen ions (H+), causing a decrease in pH in body fluids, making them more acidic. The respiratory system plays a critical role in rapidly adjusting the body’s acid–base status during and immediately after exercise, among other mechanisms.
Acids like lactic acid and carbonic acid release H+ ions, increasing the H+ concentration in body fluids and lowering the pH. To counteract the effects of excess H+, the blood and muscles contain base substances that combine with and buffer the H+ ions:
H+ + buffer → H-buffer.
Under resting conditions, body fluids have more bases (such as bicarbonate, phosphate, and proteins) than acids, maintaining a slightly alkaline tissue pH ranging from 7.1 in muscle to 7.4 in arterial blood. Arterial blood pH is tolerated within the range of 6.9 to 7.5, although extremes within this range can only be tolerated for short durations.
The pH of intra- and extracellular body fluids is regulated through chemical buffers in the blood, pulmonary ventilation, and kidney function. Major chemical buffers include bicarbonate (HCO3 –), inorganic phosphates (Pi), proteins, and hemoglobin. Bicarbonate combines with H+ to form carbonic acid, which is then converted into carbon dioxide and water in the lungs, ultimately exhaled as CO2.
The amount of bicarbonate used equals the amount of acid buffered. For instance, when lactic acid decreases pH from 7.4 to 7.0, over 60% of the initially present bicarbonate in the blood is utilized. Blood and chemical buffers are essential for transporting metabolic acids from their origin (muscles) to the lungs or kidneys, where they can be eliminated. These buffers can be recycled once H+ is transported and removed.
In muscle fibers and kidney tubules, phosphates like phosphoric acid and sodium phosphate primarily buffer H+ ions. Cells contain more protein and phosphates but less bicarbonate compared to extracellular fluids.
An increase in free H+ ions in the blood stimulates the respiratory center to increase ventilation, promoting the binding of H+ to bicarbonate and facilitating carbon dioxide removal. This leads to decreased free H+ ion concentration and an increase in blood pH. Both chemical buffers and the respiratory system counteract the acute effects of exercise acidosis.
To maintain a consistent buffer reserve, the body excretes accumulated H+ ions via the kidneys, eliminating them in urine. The kidneys filter H+ from the blood alongside other waste products, allowing for H+ elimination while maintaining extracellular bicarbonate concentration.
During sprint exercise, intense muscle glycolysis generates considerable lactate and H+, lowering muscle pH from a resting 7.1 to less than 6.7. Despite the significant production of lactate and H+ during a 400m sprint, equilibrium is reached within 5 to 10 minutes of recovery. Blood pH levels may drop to 7.10, while blood lactate concentrations can rise to 12.3 mmol/L after 5 minutes of recovery, compared to resting pH of 7.40 and lactate levels of 1.5 mmol/L.
Restoring normal blood and muscle lactate concentrations after exhaustive exercise takes 1 to 2 hours. Active recovery, involving lower-intensity exercise, facilitates quicker removal of blood lactate as it maintains elevated blood flow and enhances lactate diffusion out of muscles and lactate oxidation. Blood lactate typically returns to normal within 30 to 40 minutes after highly anaerobic exercise, thanks to chemical buffering (primarily bicarbonate) and respiratory elimination of excess carbon dioxide.
